Since this post was first published in March 2020, more research on the transmission, spread, and prevention of COVID-19 has come to light and multiple variants of the virus have infected millions of people. First there was the more virulent Delta variant, and now we are grappling with the highly transmissible Omicron variant, both of which spread much more easily than the original virus strain. Fortunately, many of the original recommendations to prevent the spread of these viruses remain the same, including smokefree requirements that eliminate the spread of respiratory droplets when someone exhales secondhand smoke or e-cigarette vapor/aerosol.
Smoking, vaping, and exposure to secondhand smoke and aerosols can increase risks associated with COVID-19 transmission. Removing face coverings to smoke or vape indoors undermines the proven benefit of face coverings and increases the risk of transmitting or inhaling COVID-19 via infectious respiratory droplets, uncovered coughs, and increased touching of faces.
More details about new evidence are continuously added in the post below, or visit our bibliography of resources related to COVID-19 and smoking/vaping.
“Businesses cannot adequately reinforce the proven risk reduction strategy of wearing face coverings while also allowing smoking… The primary mode of transmission of the virus is through person-to-person spread of respiratory droplets. As people remove face coverings to smoke or vape, they are exhaling respiratory droplets over a longer distance. The act itself requires individuals to more frequently touch their face and mouths – another direct contradiction to recommended COVID-19 prevention strategies.”
Many businesses, schools, and communities are once again requiring masks in response to the increase in positive case rates as a result of the impact of the Delta and Omicron variants. It is impossible to maintain mask wearing while allowing indoor smoking since people need to remove their masks to smoke. Now is not the time to expose workers and patrons to secondhand smoke and COVID-19.
Vaccination is the best way to prevent infection and slow the spread of COVID-19, including the Delta and other variants. The following public health measures provide additional best practice recommendations to help mitigate or prevent the spread of COVID-19.
- Wear a Mask.
- Avoid large gatherings, meet outside, and be sure to socially distance from others.
- Do not go out in public if you feel sick.
- Wash your hands frequently with soap and water.
- Avoid exposure to or contributing to the spread of respiratory droplets and aerosols (e.g., use a tissue to cover coughs and sneezes, sneeze into your elbow; if you smoke or vape, take it outside, away from others).
- Prevent exposure to secondhand smoke and e-cigarette aerosol or vape by adopting a smokefree policy with no smoking or vaping indoors. Move smoking to socially distanced outdoor areas away from entrances.
COVID-19 reminds us that health prevention policies matter greatly.
Our thoughts are with everyone impacted by coronavirus, including front-line healthcare workers as well as workers in the hospitality and entertainment industries who are generally the least likely to have paid sick leave and health care coverage, and too many of whom are still working in smoke-filled environments.
Just as social distancing and handwashing help prevent the spread of disease, eliminating secondhand smoke is critical to prevent acute and chronic diseases, and to save lives by reducing the risk of heart disease, stroke, respiratory diseases, and lung cancer by up to 30% at a population-wide level.
Secondhand Smoke Exposure
Research recently published in the journal Health Promotion and Chronic Disease Prevention in Canada points to the inequity in impact of the current pandemic on marginalized groups; the same groups that are more likely to smoke and be exposed to secondhand smoke at work. One of the recommended strategies to protect these priority populations is the passage of comprehensive smokefree policies. This is the work that ANR/F is supporting in communities and states across the country to close gaps in smokefree protections and maintain gains by turning temporary 100% smokefree indoor air protocols into permanent policy change.
The Nicotine and Cannabis Policy Center at UC Merced highlights evidence about COVID-19, tobacco and vaping, including risks to children exposed to secondhand smoke, finding that “Kids exposed to secondhand smoke have weakened immune systems and higher chances of complications from pneumonia.” Since COVID-19 attacks the respiratory system, it is critical to prevent exposure to anything that would weaken the lungs.
Worksites that still allow indoor smoking continue to create a health risk, especially in the time of COVID-19. Just like coronavirus, secondhand smoke spreads throughout buildings. Casino, bar, and hotel ventilation systems do not eliminate exposure to the gases, toxins, carcinogens, and particulate matter contained in secondhand smoke and e-cigarette aerosol.
Sadly, more than 100 Americans die every day from secondhand smoke exposure. Casino and hospitality workers are the workforce with the most exposure to secondhand smoke, but it’s a health hazard for everyone in a building with smoking. Exposure to secondhand smoke is a health risk we can eliminate by closing gaps in smokefree protections for all workplaces, public places, and multi-unit homes. Powerful corporate interests, including tobacco companies, want to enable indoor smoking in venues like bars, music venues, and casinos as a way to maximize smoking profits and keep people addicted to tobacco and other nicotine products.
Community Public Health experts and advocates must continue their efforts to prevent rollbacks to smokefree protections, and attempts to preempt local authority to enact smokefree and other tobacco-related laws, in order to protect health and prevent another generation from becoming addicted to nicotine products.
Secondhand smoke causes underlying health conditions – a risk factor for more severe COVID symptoms
Exposure to secondhand smoke makes breathing difficult, and is also a significant risk factor for many underlying health conditions linked with more severe COVID-19 disease, including heart disease, diminished lung function, and associated risk of respiratory illnesses. Those who are considered high-risk and susceptible to virus exposure will need to do their best to avoid smoke-filled environments. Survivors of COVID-19 experiencing lung damage will also need to avoid secondhand smoke.
Secondhand smoke damages the immune system – a risk factor for more severe COVID symptoms
Secondhand smoke damages the immune system as evidenced by the nation’s doctor, the U.S. Surgeon General. According to the 2014 Surgeon General’s Report, there is sufficient evidence to infer that cigarette smoke exposure compromises the immune system and immune homeostatis, which increases risk for several disorders, including pulmonary infection. Available science from the 2006 and 2010 Surgeon General Reports shows that the profile of secondhand smoke is largely consistent with that of primary smoke inhaled into the lungs from an active smoker. The effect would be expected to be smaller for secondhand compared to primary exposure given volume of toxicants and length of exposure. The potential role of the immuno-compromising nature of secondhand smoke is further reinforced by emerging research that has specifically documented a link between the two.
Only 100% smokefree environments can guarantee protection to employees and patrons from the toxins in secondhand smoke. Ventilation systems do not address the health hazards of secondhand smoke. These systems cannot eliminate exposure to the gases, toxins, carcinogens, and particulate matter contained in secondhand smoke and e-cigarette aerosol. Even during brief or low levels of exposure, secondhand smoke still creates significant health risks, especially to the cardiovascular system. There is no safe level of exposure to secondhand smoke. The effects of secondhand smoke exposure on the body are immediate and can produce adverse inflammatory and respiratory effects within 30 minutes of exposure.
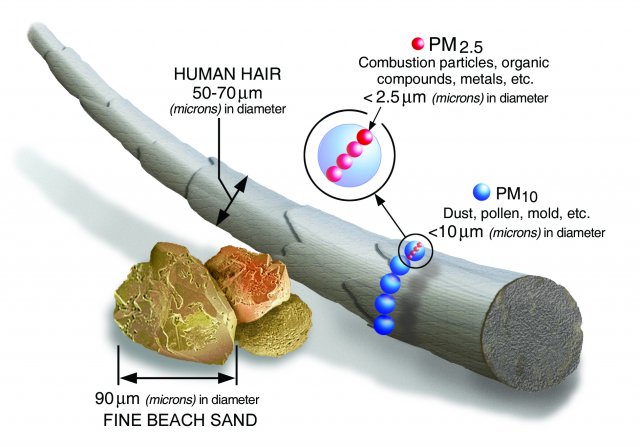
Evidence about transmission through aerosols and respiratory droplets: Aerosol transmission (sometimes referred to as airborne transmission) is similar to droplet transmission, except that the bits of fluid are so small that they can linger in the air for minutes to hours. To understand the scale of aerosols, the diameter of a human hair is about 80 microns, and aerosols smaller than about 50 microns can float in the air long enough to be inhaled. SARS-CoV-2 is only 0.1 microns in diameter, so there is room for plenty of viruses in aerosols.
According to the CDC, the principal mode of transmission of COVID-19 is through exposure to respiratory fluids. One of the most common means of exposure to respiratory fluids is through inhalation of fine respiratory droplets and aerosols. People naturally release respiratory fluids through droplets that are released when exhaling when breathing, speaking, coughing, sneezing or smoking.
COVID-19 and what we can do to minimize risk factors
The Centers for Disease Control has guidance on preventing risks for Coronavirus or COVID-19 and outlining which populations are most at risk for getting COVID-19: “Older adults and people who have severe underlying chronic medical conditions like heart or lung disease or diabetes seem to be at higher risk for developing more serious complications from COVID-19 illness. Please consult with your health care provider about additional steps you may be able to take to protect yourself.”
While young adults are at a lower risk, there are health risk factors that can lead to susceptibility to the virus, including smoking and exposure to secondhand smoke. Smoking leads to respiratory illnesses: everything from bronchitis to asthma to COPD and lung cancer. Therefore, individuals who smoke tobacco or marijuana, and potentially those who vape electronic smoking devices, reduce their lung function by introducing particulate matter, toxins, and carcinogens into their lungs, which then increases susceptibility for respiratory illnesses. In addition, secondhand smoke exposure is similarly associated with diminished lung function and illnesses, and therefore also a risk factor for susceptibility to viruses like COVID-19. We encourage individuals, particularly those who are considered high risk and susceptible to virus exposure, to do their best to avoid smoke-filled indoor environments.
[See summary of the evidence on the respiratory effects of e-cigarettes and the ways that e-cigarettes impair lungs’ ability to fight off infections.]
Given these risk factors, those that choose to smoke are encouraged to consider quitting for good. We know that it is incredibly challenging to quit, particularly during stressful times, and that stress often leads to relapse among former smokers. That’s not by accident. The tobacco industry intentionally made cigarettes more addictive and through their understanding of nicotine’s addictive impact on brain chemistry knew it would be extremely difficult for users, their core customers, to quit. If you want to quit, you are not alone—there are many FREE resources, online and by phone, that can help people who wish to quit.
For businesses, now is the perfect time to go smokefree for good. Restaurants, bars, and casinos have nimbly responded to ongoing challenges presented by the pandemic. A 100% smokefree environment is an essential component of ensuring employees feel safe at work and customers can enjoy the environment without concern for their health and safety. In addition to the deep cleaning to disinfect against germs and viruses, consider the tobacco smoke residue, including gases, toxins, carcinogens, and particulates, left in the air, on walls and surfaces, and in carpets and draperies.
Airports are also closing their smoking rooms to prevent the spread of COVID-19. We strongly urge any airport that still has a smoking room or lounge to permanently prohibit smoking inside the airport. Smoking rooms do not protect people from the health hazards caused by secondhand smoke exposure. Smokefree air is important for travelers and workers at all times, not only during a health emergency. Going smokefree is easier than you think, and we’ve outlined the steps to help you in the process.
We strongly encourage businesses to maintain 100% smokefree environments.
Early findings from Italy and China demonstrate that those who contracted COVID-19 and recovered still show signs of diminished lung function. Therefore exposure to other, ongoing risk factors, including secondhand smoke, could result in relapse or some other lung-related illness.
Coronavirus has brought into sharp focus the health impact of breathing shared air in workplaces and public gathering places such as casinos, bars, and cruise ships. The still-unfolding COVID-19 crisis shows that businesses are materially impacted by population health risk factors and the urgent need to rethink old assumptions about the health and economic benefits of going smokefree.
Smokefree air protects the health and safety of workers along with those who have respiratory and cardiovascular illnesses. Smokefree air will help keep the air safe and welcoming in hospitality and entertainment workplaces for everyone.
Additional Information:
Smoking Doubles the Mortality Risk in COVID-19: A Meta-Analysis of Recent Reports and Potential Mechanisms (Added November 20, 2020)
COVID in the U.S.: Latest Map and Case Count (Added November 5, 2020)
COVID-19 transmission through aerosols (Added August 28, 2020)
COVID-19, TOBACCO & VAPING INFORMATION from the Nicotine and Cannabis Policy Center at UC Merced (Added August 28, 2020)
Children, COVID-19 and Secondhand Smoke graphic (Added August 28, 2020)
1 in 3 young adults vulnerable to severe Covid-19 — and smoking plays a big part, research finds (Added July 15, 2020)
Patients with underlying conditions were 12 times as likely to die of covid-19 as otherwise healthy people, CDC finds (Added July 15, 2020)
WHO Statement: Tobacco Use and COVID-19 (Added 5/13/2020)
Second Open Letter About COVID-19 and LGBTQ+ Communities (Added 4/24/2020)
Almost 90% of COVID-19 Admissions Involve Comorbidities (Added 4/16/2020)
*This post was originally published on March 18, 2020, and is being updated as new information and resources become available.